Tuberculosis (TB)
Tuberculosis (TB) is a chronic bacterial infection caused by Mycobacterium tuberculosis. It is one of the world’s oldest and most widespread infectious diseases, primarily affecting the lungs but capable of involving other parts of the body such as the kidneys, brain, and spine. Despite being preventable and treatable, TB remains a significant global health challenge, particularly in low- and middle-income countries.
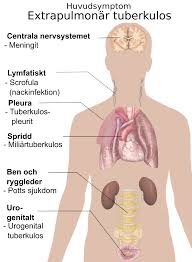
Table of Contents
Key Features of Tuberculosis
1. Transmission
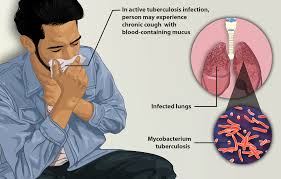
TB spreads through the air when an infected person with active pulmonary TB coughs, sneezes, or speaks, releasing microscopic droplets that contain the bacteria. Prolonged exposure is usually required for transmission, making it more common in households, workplaces, or other crowded settings.
2. Types of TB
- Latent TB: The bacteria remain in the body in an inactive state, causing no symptoms. Latent TB is not contagious but can activate if the immune system becomes compromised.
- Active TB: The bacteria multiply and cause symptoms. This form is contagious and can spread to others.
3. High-Risk Groups
Individuals at greater risk of developing TB include:
- People with weakened immune systems (e.g., those with HIV/AIDS, diabetes, or undergoing chemotherapy).
- Malnourished individuals.
- Smokers and those with substance use disorders.
- Healthcare workers and individuals in close contact with TB patients.
Symptoms of Tuberculosis
Pulmonary TB (Affects the Lungs):
- Persistent cough lasting more than three weeks.
- Chest pain or discomfort.
- Coughing up blood or phlegm.
- Fatigue and weakness.
- Unexplained weight loss.
- Fever and chills.
- Night sweats.
Extrapulmonary TB (Affects Other Organs):
- Symptoms vary depending on the affected organ. For example:
- Spinal TB: Back pain and stiffness.
- Renal TB: Blood in urine.
- Brain TB (Tuberculous meningitis): Headache, confusion, and seizures.
Diagnosis of Tuberculosis
Timely diagnosis is critical for effective treatment and controlling the spread of TB. Common diagnostic methods include:
1. Skin Test (Tuberculin Skin Test/ Mantoux Test):
- A small amount of tuberculin is injected under the skin. The injection site is checked after 48-72 hours for swelling or induration. A positive result indicates TB exposure but does not confirm active disease.
2. Blood Tests:
- Interferon-gamma release assays (IGRAs) detect TB infection by measuring the immune response to TB bacteria.
3. Chest X-ray:
- Used to detect abnormalities in the lungs that may suggest TB infection.
4. Sputum Test:
- Analysis of sputum samples to detect Mycobacterium tuberculosis. Molecular tests like GeneXpert can also identify drug-resistant strains.
5. Advanced Imaging and Biopsy:
- CT scans or MRI for extrapulmonary TB.
- Biopsy of affected tissues for microscopic examination.
Also Read: https://coveragezone31.com/hair-loss
Treatment of Tuberculosis
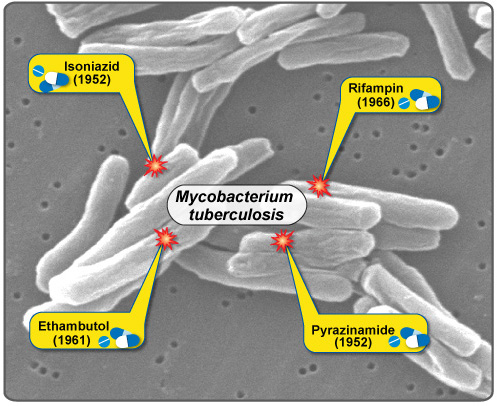
1. Standard TB Treatment Regimen:
The treatment for TB typically involves a combination of antibiotics over an extended period to ensure complete eradication of the bacteria and prevent drug resistance. The standard regimen includes:
- Intensive Phase (First 2 Months):
- Four drugs: Isoniazid, Rifampin, Pyrazinamide, and Ethambutol.
- Continuation Phase (Next 4-7 Months):
- Two drugs: Isoniazid and Rifampin.
2. Drug-Resistant TB:
Some strains of Mycobacterium tuberculosis have developed resistance to standard drugs:
- Multidrug-Resistant TB (MDR-TB): Resistant to Isoniazid and Rifampin. Treated with second-line drugs like fluoroquinolones and injectable agents (e.g., amikacin).
- Extensively Drug-Resistant TB (XDR-TB): Resistant to multiple first- and second-line drugs. Requires specialized treatment regimens and prolonged therapy.
3. Directly Observed Treatment, Short-Course (DOTS):
- A strategy recommended by the World Health Organization (WHO) to ensure patient compliance.
- Healthcare providers or trained individuals observe patients taking their medications.
4. Adjunctive Treatments:
- Nutritional Support: Malnutrition weakens the immune system; a balanced diet aids recovery.
- Treatment of Co-Infections: Addressing conditions like HIV/AIDS improves outcomes.
Prevention of Tuberculosis
1. Vaccination:
- The Bacillus Calmette-Guérin (BCG) vaccine is commonly administered in high-burden countries to prevent severe TB forms in children.
2. Early Detection and Treatment:
- Prompt identification and treatment of active TB cases reduce transmission.
3. Infection Control Measures:
- Use of masks, proper ventilation, and air filtration in crowded settings.
- Isolation of contagious patients during treatment.
4. Preventive Therapy:
- Individuals with latent TB may receive prophylactic treatment to prevent activation, especially in high-risk groups.
Global Burden of Tuberculosis
According to the WHO, TB remains one of the top 10 causes of death worldwide. Key statistics include:
- Approximately 10 million people develop TB annually.
- Over 1.5 million TB-related deaths occur each year.
- Drug-resistant TB poses a growing challenge, with MDR-TB cases increasing in many regions.
Advancements in TB Management
Recent developments are helping combat TB more effectively:
- Rapid Diagnostic Tools: GeneXpert and line-probe assays for faster, more accurate detection.
- Shorter Treatment Regimens: Research is underway to reduce the duration of TB treatment.
- New Vaccines: Trials for more effective TB vaccines are in progress.
- Digital Tools: Apps and technologies to track treatment adherence and patient progress.
Conclusion
Tuberculosis is a preventable and treatable disease, but it requires global cooperation and resources to address its burden. Early diagnosis, proper treatment, vaccination, and public health initiatives are crucial in reducing TB incidence and mortality. Continued investment in research and innovation can pave the way for a TB-free world. Source https://pmc.ncbi.nlm.nih.gov/