Status and Challenges for Tuberculosis (TB) Control in India:
Introduction:
Tuberculosis (TB) is infectious disease caused by predominantly by Mycobactrium Tuberculosis. Tuberculosis is most commonly Transmitted by inhalation of infected droplet nuclei which are discharged in the air when infected patient sneezes. TB disease usually affects the lungs, but is can also involve other parts of the body. Pulmonary TB which affects lungs is an infectious form of the disease. Extra pulmonary TB can affects the lymph nodes, the pleura, Bones and joints, the Genito-urinary tract and nerve system.
India has the highest burden of tuberculosis (TB) globally, accounting for about 27% of global TB cases and deaths, as per the World Health Organization’s Global TB Report. While significant progress has been made in TB control, the country continues to face numerous challenges that hinder the elimination of the disease. Here’s an analysis of the current status and challenges from the perspective of key stakeholders:
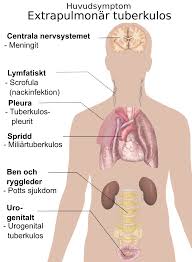
Table of Contents
Status of Tuberculosis (TB) Control in India
- National TB Elimination Program (NTEP):
Formerly known as the Revised National Tuberculosis Control Program (RNTCP), the NTEP aims to eliminate TB by 2025, five years ahead of the global target.- Implementation of universal drug-susceptibility testing.
- Active case-finding campaigns to identify undiagnosed cases.
- Free diagnostics and treatment through public health infrastructure.
- Improved Diagnostics:
- Availability of rapid molecular diagnostics like GeneXpert and Truenat in most districts.
- Expansion of sputum microscopy centers and digital radiology.
- Private Sector Engagement:
- Inclusion of private healthcare providers under the NTEP for notification of TB cases.
- Public-private partnerships for free TB treatment and diagnostics.
- Social Support Initiatives:
- Introduction of schemes like Nikshay Poshan Yojana, providing nutritional support to TB patients.
- Financial incentives for treatment adherence. https://dghs.gov.in/content/1358_3_RevisedNationalTuberculosisControlProgramme.aspx

Challenges in Tuberculosis (TB) Control in India
1. Diagnostic and Reporting Gaps
- Underreporting: A large proportion of Tuberculosis (TB) cases remain undiagnosed or unreported, especially in rural areas and among marginalized communities.
- Limited Access: Despite improved diagnostics, access to high-quality testing remains limited in remote areas.
- Delays in Diagnosis: Many patients approach informal healthcare providers first, leading to delayed diagnosis and treatment.
2. Drug-Resistant TB (DR-TB)
- India reports a high burden of multidrug-resistant Tuberculosis (TB) (MDR-TB) and extensively drug-resistant TB (XDR-TB).
- Misuse of antibiotics, incomplete treatments, and lack of drug adherence contribute to resistance.
- Second-line drugs are expensive, require longer treatment, and have significant side effects, discouraging adherence.
3. Stigma and Awareness
- Social stigma surrounding Tuberculosis (TB) prevents many patients from seeking care or completing treatment.
- Awareness campaigns have yet to reach rural and tribal populations effectively.
4. Health System Challenges
- Overburdened healthcare infrastructure, particularly in public hospitals.
- Shortages of skilled personnel, such as microbiologists and DOTS providers.
- Inefficient supply chain management leading to delays in medicine delivery.
5. Socioeconomic Factors
- Poverty, malnutrition, and overcrowded living conditions contribute to the spread of TB.
- Migrant populations and urban slums pose challenges for continuity of care.
6. Funding Gaps
- While government funding for Tuberculosis (TB) control has increased, the resources allocated are insufficient to meet the ambitious 2025 elimination target.
- Dependence on international funding from agencies like the Global Fund creates vulnerabilities.
7. Co-morbidities
- HIV-TB Co-infection: India has a high number of TB-HIV co-infected patients, complicating treatment outcomes.
- Diabetes and TB: The growing diabetes epidemic in India is increasing TB susceptibility and complicating its management.
Also Read:https://coveragezone31.com/tuberculosi
Stakeholders’ Perspectives
1. Government
- Priorities: Achieving the 2025 TB elimination target through active case finding, universal testing, and adherence monitoring.
- Challenges: Limited coordination between central and state governments and competing public health priorities.
2. Healthcare Providers
- Role: Early diagnosis, effective treatment, and patient follow-up.
- Challenges: Overwhelming patient loads, inadequate training, and reluctance in the private sector to notify TB cases due to stigma or fear of government oversight.
3. Patients and Communities
- Role: Adherence to treatment and awareness of symptoms.
- Challenges: Stigma, lack of education, and financial constraints limit access to care.
4. NGOs and Civil Society
- Role: Advocacy, community engagement, and providing support services to marginalized populations.
- Challenges: Dependence on government or donor funding and lack of scalability of initiatives.
5. International Organizations
- Role: Technical assistance, funding, and policy guidance (e.g., WHO, Global Fund).
- Challenges: Ensuring sustainability and alignment with local needs.

Way Forward
1. Strengthening Health Infrastructure
- Invest in TB-specific healthcare facilities and train healthcare workers to manage complex TB cases.
- Expand the reach of diagnostic tools, especially in rural and tribal areas.
2. Innovations in Treatment
- Develop and deploy shorter, more effective treatment regimens for drug-resistant TB.
- Ensure timely availability of new drugs like bedaquiline and delamanid.
3. Community Engagement
- Increase public awareness campaigns to reduce stigma and encourage early diagnosis.
- Engage local leaders and influencers to promote TB-related health education.
4. Policy and Governance
- Strengthen public-private partnerships to ensure seamless TB case notification and treatment delivery.
- Integrate TB services with other public health programs like HIV and diabetes care.
5. Enhanced Funding
- Allocate higher domestic funding for TB programs to reduce reliance on international donors.
- Explore corporate social responsibility (CSR) initiatives to fund TB-related activities.
6. Research and Development
- Focus on developing more effective vaccines and rapid diagnostic tools.
- Encourage operational research to tailor strategies to local needs.
Conclusion
TB control in India is at a critical juncture. While efforts under the NTEP have shown promise, achieving elimination by 2025 requires addressing systemic challenges, increasing community involvement, and strengthening the healthcare infrastructure. A multisectoral approach involving government, healthcare providers, communities, and international partners is essential to overcome barriers and achieve the goal of a TB-free India.